Staphylococcus aureus, a frequent colonizer of the skin and nasal mucosa of humans and animals, is a highly successful opportunistic pathogen.
Major Characteristics ofStaphylococcus aureus
- Gram stain: Staphylococci appear as Gram-positive cocci that occur singly and in pairs, tetrads, short chains, and irregular grape-like clusters
- Catalase Test: Positive
- Coagulase Test: Positive
- Non-motile
- Non-sporing
- Often unencapsulated or have a limited capsule
- Facultative anaerobes.
Main diseases caused byStaphylococcus aureus
Mneomonic:Diseases caused byStaphylococcuscan be remembered using this acronym “SOFTPAINS”
- Skin Infections & Surgical wound infections
- Osteomyelitis
- Food poisoning/gastroenteritis
- Toxic shock syndrome
- Pneumonia (mainly hospital-acquired)
- Acute endocarditis
- Infective arthritis
- Necrotizing fasciitis
- Sepsis and Staphylococcal scalded skin syndrome (SSSS)
Virulence factors ofS. aureus
- Surface proteins: Protein A (prevents activation of complement), clumping factor, teichoic acid (adherence and induction of septic shock)
- Superantigens: Enterotoxin A-D, Exfoliatin A&B, Toxic Shock Syndrome Toxin (TSST)-superantigen.
- Cytotoxins: α-hemolysin, β-hemolysin,γ-hemolysin, δ-hemolysin, Panton-Valentine Leukocidin (PVL), Exfliatin (epidermolytic-cleaves desmoglein in desmosomes)
- Enzymes: Nuclease, lipase, hyaluronidase, coagulase (causes plasma to clot), staphylokinase, glycerol ester hydrolase, catalase (degradation of H2O2 limits the ability of neutrophils to kill *S. aurues),*etc.
Laboratory diagnosis
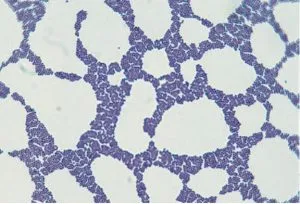
- Gram staining: Gram-positive cocci in clusters, cocci may appear singly in pairs or in short chains.
- Culture
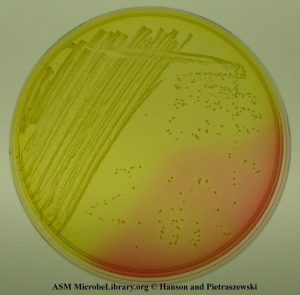
Blood Agar: growth occurs abundantly within 18 to 24 hours, yellow or golden yellow colonies with or without Beta hemolysis are seen. Mannitol Salt Agar (MSA) is a selective media commonly used for the isolation of S. aureus. After inoculation, MSA plates were incubated at 35°C for 24 to 48 hours. S. aureus is mannitol fermenting bacteria and gives yellow or gold colonies.
- Biochemical tests:
Catalase test: Positive Coagulase test: Positive- DistinguishS. aureus from coagulase-negative Staphylococcus aureus (CONS). CONS are further differentiated on the basis of novobiocin sensitivity test ( S. epidermidis is sensitive, whereas S. saprophyticus is resistant).
Biochemical tests for the identification ofS. aureus
| Name of the test | Staphylococcus aureus | Notes |
|---|---|---|
| Catalase test | Positive | To differentiate staphylococci from streptococci. |
| Hemolysis | β-hemolysis or non-hemolysis | |
| Coagulase test | Positive | To differentiate S. aureus from CONS. |
| Mannitol fermentation | Yes | To differentiate S. aureus (fermenter) from CONS (non-fermenter) |
| Furazolidone disk Test | Sensitive | To differentiate staphylococci from micrococci (resistant) |
| Polymyxin B sensitivity test | Resistant | Most staphylococcal species are susceptible to polymyxin B, but S. aureus, S. lugdunensis, and S. epidermidis are resistant. |
| Bacitracin( 0.04-U disk) susceptibility test | Resistant | To separate staphylococci from micrococci (susceptible) |
| Microdase test | Negative | To differentiate staphylococci from micrococci. |
| DNase test | Positive | To differentiate S.aureus from other Staphylococci (-ve) when coagulase test is unavailable. |
Antimicrobial Resistance
Staphylococcus aureus, including Methicillin-resistantStaphylococcus aureus(MRSA), is one of the most common causes of healthcare-associated infections. The first report of Vancomycin-Resistant Staphylococcus aureus(VRSA)**came in 2002. VRSA is also resistant to methicillin and other classes of antibiotics, limiting the available treatment options.
References
- Forbes, S., Sahm, D. F., & Weissfeld, A. S. (2002). Bailey & Scott’s Diagnostic Microbiology. Mosby.
- Foster, T. (1996). Staphylococcus. In S. Baron (Ed.), Medical Microbiology. (4th ed.). University of Texas Medical Branch at Galveston.
- Tong, S. Y., Davis, J. S., Eichenberger, E., Holland, T. L., & Fowler, V. G., Jr (2015). Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clinical microbiology reviews, 28(3), 603–661. https://doi.org/10.1128/CMR.00134-14