Campylobacter usually causes diarrhea (often bloody). It is the most common cause of gastroenteritis worldwide, enterocolitis, especially in children. It causes systemic infection (rarely) in children and debilitated adults. Systemic infections (bacteremia), mostly by Campylobacter intestinalis.
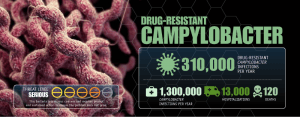
Drug-resistant Campylobacter is one of the top 18 drug-resistant threats to the United States. CDC has categorized it under “Serious concern”.
Important properties ofCampylobacter jejuni
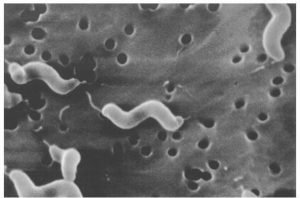
- Curved, gram-negative rods that appear either comma or S-shaped.
- Microaerophilic (growing best in 5% oxygen rather than in the 20% present in the atmosphere): More info about the oxygen requirements of bacteria
- Campylobacter jejuni grows well at 42°C
- Oxidase positive
- Posses amphitrichous (bipolar) flagella
Disease Transmission
- Source: Cattle, chicken, dogs, etc
- Mode of transmission: Faecal-oral route {food (milk or meat products) and water contaminated with animal feces}. Human to human transmission can occur but is less frequent.
Reservoir of infection: Domestic animals such as cattle, chickens, dogs, etc.
Campylobacteriosis
- Symptoms (within 2-5 days of exposure):
Watery foul-smelling diarrhea (may be bloody) nausea and vomiting (may be seen) cramping severe abdominal pain and fever
- Can be treated with antibiotics
- Usually, self-limiting disease that typically lasts about one week.
- Some infected persons do not have any symptoms.
Campylobacterinfections are also associated with some autoimmune diseases:
- Guillain-Barré syndrome
- Reactive arthritis
- Reiter’s syndrome
Guillain-Barré Syndrome
GI infection with C. jejuniis associated with Guillain-Barré syndrome
- Most common cause of acute neuromuscular paralysis
- Autoimmune disease
- 40% caused by C. jejuni infection
- Formation of antibodies against C. jejuni that cross-reacts with antigens on neurons.
- Immune system attacks its own nerves; axons are attacked by antibodies against the bacteria C. jejuni, which react with proteins of the peripheral nerves.
Reactive arthritis (Reiter’s syndrome)
- Infection with C. jejuni is also associated with reactive arthritis (Reiter’s syndrome)
- Painful swelling of joints often the knees and/or ankles.
- Other bacteriae.g., Chlamydia trachomatis, Salmonella, Shigella, Yersiniaalso cause reactive arthritis.
Pathogenesis
Campylobacter jejuni produces enterotoxins and cytotoxins.
Laboratory diagnosis
Specimen: Diarrhoeal or a dysenteric specimen containing blood, pus, and mucus. If immediate processing is not feasible specimen can be refrigerated up to 24 hours before culture as the organism are resistant to cold temperature.
- Blood agar plate containing antibiotics (to inhibit the fecal flora) is the media of choice. Inoculated plates are incubated at 42°C in a microaerophilic atmosphere containing 5% oxygen and 10% carbon dioxide.
- Failure to grow at 25**°**C
- Oxidase test: positive
- Catalase test: Positive
- Sensitive to Nalidixic acid
Note: Campylobacter intestinalis does not grow at 42**°C, but grows at 25°**C and is resistant to nalidixic acid.
Drugs of choice for Campylobacter infection: Erythromycin or ciprofloxacin is used successfully inCampylobacter jejuni enterocolitis.
References
- Altekruse, S. F., Stern, N. J., Fields, P. I., & Swerdlow, D. L. (1999). Campylobacter jejuni–an emerging foodborne pathogen. Emerging infectious diseases, 5(1), 28–35. https://doi.org/10.3201/eid0501.990104
- Young, K. T., Davis, L. M., & Dirita, V. J. (2007). Campylobacter jejuni: molecular biology and pathogenesis. Nature reviews. Microbiology, 5(9), 665–679. https://doi.org/10.1038/nrmicro1718